Gastric bypass surgery
Preparation for surgery:
Face-to-face consultation (and telephone consultation before this) with the bariatric surgeon.
Necessary examinations: laboratory, EKG, echocardiogram, abdominal ultrasound, chest X-ray, gastroscopy, psychologist and anesthetist consultation. These can also be done at your local hospital, but the Duna Medical Center is happy to help you.
For 2-4 weeks before surgery, a so-called 'liver-shrinking' diet. The purpose of this is to improve conditions in which to carry out the operation. The diet is a low-carbohydrate, 1,200 kcal/day diet prepared by our dietician.
On the evening before surgery, being given an anti-coagulation injection (at the Duna Medical Center or at home).
On the day of the operation:
Administrative admission to the surgery department of the Duna Medical Center. The operation lasts 90-120 minutes, under anesthesia. There are no catheters, no tubes, the wounds are sutured with absorbable sutures. 4 hours after awakening, the patients get up and go to the toilet, with assistance. Additional mobilization every 2 hours. At night, we use a compression foot pump, which is the most effective tool against the formation of a hematoma.
1st day after surgery:
Specialist visit. If there is no problem, fluid intake can be started orally. Blood test check.
2nd day after surgery:
Specialist visit. If everything goes according to plan, the final report will be issued and you will leave the Surgery Department of the Duna Medical Center.
A blood thinner injection is required for another 10 days. Planned specialist check-up in 6-8 weeks. We will send a detailed description of the post-surgery follow-up to your general practitioner, but if required, the private general practitioner of the Duna Medical Center is also available to carry it out.


Unsure what to do after surgery?
Please watch this:
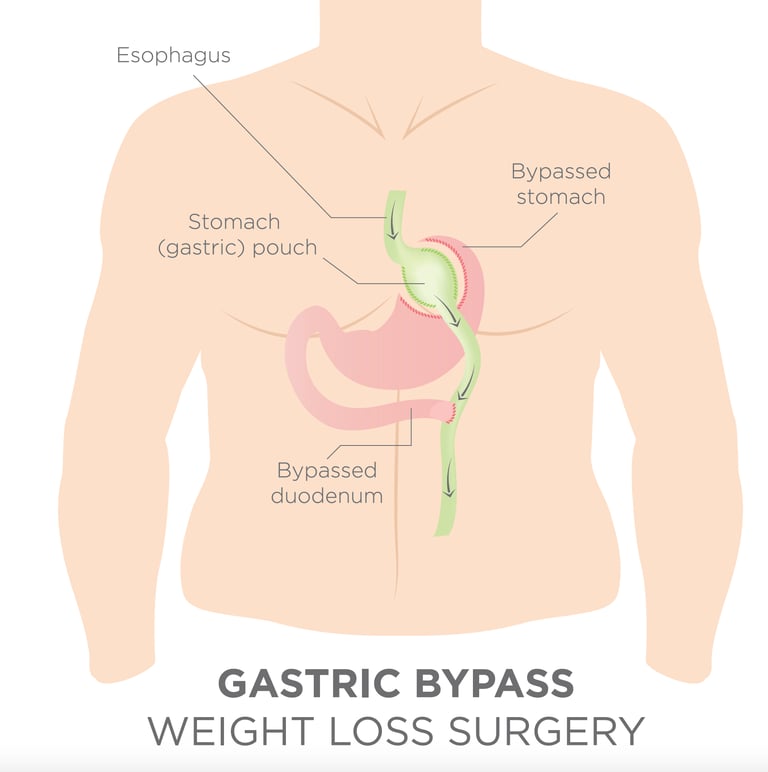
Roux-en-Y gastric bypass (RYGB), commonly called simply “gastric bypass”, is one of the most commonly performed bariatric procedures worldwide and has long been considered the “gold standard” of bariatric surgery. The gastric bypass was first written about in 1967 and was performed as open surgery for several decades. However, since the 1990s, it is almost entirely performed by the laparoscopic (keyhole) approach. The operative procedure involves staple-dividing the stomach into two chambers. The upper chamber – called the pouch – receives food and is very small, holding about 20-30 cc. The lower chamber – called the gastric remnant – is “bypassed” and does not receive food. The small intestine is divided at a certain point and one end is connected (“anastomosed”) to the pouch. A second connection (“anastomosis”) is made to connect the disconnected stomach and duodenum to the small bowel. This connection enables the digestive fluids to meet the ingested food to enable nutrient breakdown and absorption. The distance between the two connections can vary by surgeon preference but is generally 50 to 150 cm. After the procedure is completed, food advances directly from the small gastric pouch to the small intestine without passing through the lower portion of the stomach, duodenum and upper small bowel (jejunum). This gastric bypass is thought to help obese people lose weight in several different ways. The small pouch restricts the amount of food that can be eaten. The connection between the small bowel and the gastric pouch re-routes the transit of food directly into the small bowel. Since the food does not go through the bypassed portion of the stomach and duodenum there is less absorption that takes place. There are further metabolic and hormonal changes that lead to reduced appetite and an increased feeling of fullness.
Mr Vasas has a personal experience of more than 720 RYGB procedures (figure up to and including Oct 2022) acting as a primary surgeon, and has a rate of zero for both incidents of anastomotic leak and mortality. All his surgery data is uploaded onto the National Bariatric Surgery Registry and is publicly accessible .
The procedure of the gastric bypass
Following bypass surgery patients can expect to lose around one third of their total body weight or 70 to 75% of the original excess weight. The usual weight loss is 6 kg (1 stone) per month. The maximum effect on weight loss is normally observed during the first two years. There is typically some weight regained but most studies suggest that most patients maintain a weight loss of around 25% beyond 10 years. In addition to weight loss, several obesity-related conditions will typically improve after surgery. These include type 2 diabetes, hypertension, dyslipidemia, metabolic syndrome, "fatty liver disease", and obstructed sleep apnea. In fact, almost 80% of patients with type 2 diabetes will experience normalisation of their blood sugar levels and will either be off all of their anti-diabetic medication or require markedly less medication. At centres that do a large number of bariatric procedures each year, the risk of postoperative complications is low. The risk of dying from the surgery is less than 0.2% and the risk of severe complications such as bleeding, infections and thromboembolism is less than 5%. Gastric bypass surgery is currently as safe as gallbladder surgery. However, the gastric bypass procedure can result in significant vitamin and mineral deficiencies including Iron, vitamin B12, vitamin B1, calcium, zinc, vitamin D and folate. Therefore, as with all bariatric procedures, the patients who undergo gastric bypass require life-long surveillance and vitamin and mineral supplementation.




